Dispatches From the Front Lines
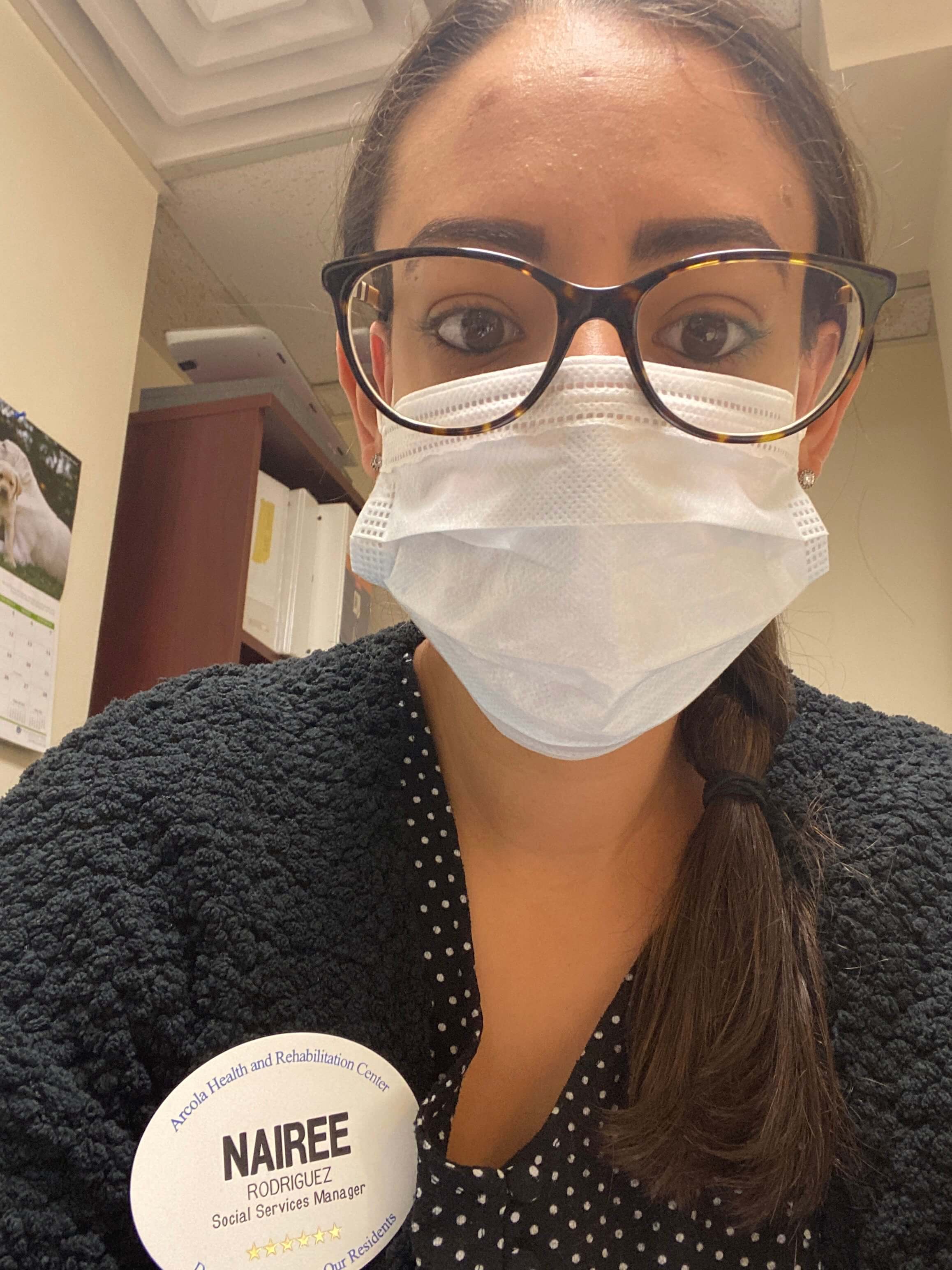
Nairee Rodriguez earned her master’s degree in social work in 2018. She is the social services director at Arcola Health and Rehabilitation in Silver Spring, Maryland. She spoke with us about what her experience has been like working at a facility that serves both short- and long-term care patients during the height of the COVID-19 pandemic.
When we all went into health care, I don’t think anybody ever expected anything like this to happen, so we’ll say “this is what we signed up for,” but we truly did not sign up for something like COVID-19.
At Arcola Health and Rehabilitation Center in Silver Spring, Maryland, we provide short-term skilled nursing for patients in need of physical and occupational therapy, but we’re largely a nursing home, a place where patients who require long-term care can live out their remaining days.
We’re a 140-bed facility but we’ve dropped down to 121 patients since COVID-19 began. I kind of hold my breath in the morning until we get our reports in to see who has passed. It’s been really rough because some of our staff has been with us for 25 to 40 years and they get very attached to the patients, especially those who have been with us for a long time.
Right now in the social work department, it’s just me and my assistant sharing four units. I handle the short-term care and dementia units.
Under normal circumstances, we would be taking in three to five admissions per day, we’d do our assessments, we’d make a care plan and discuss it with the patients and their families, schedule home health care, and conduct discharges. We still do all of that but our care plans are dramatically different.
We call our families every week to give an update. About 87 percent of our residents can’t make calls on their own, so we have also been scheduling FaceTime calls with their families once or twice per week.
Through this, we’re getting closer with families, which makes it even harder when someone passes. I feel like you don’t really deal with it at first because you’re just going through the motions and have a million things to do, but I do feel like this is going to lead to some post-trauma.
Everything has been so hard on the patients. The people who are here long term are already kind of depressed because they can’t be home, so even something as simple as not being able to leave the hallways when they’re walking in the building is making it tougher on them.

We have an amazing activities department, and we’ve been trying to offer as many activities as possible. We do Bingo by yelling the numbers up and down the hallways. We do cookouts once a week, hand out crossword puzzles and coloring books every day, and have a musician here twice a week to play for the residents.
There are some patients, like those in our dementia unit, who don’t really understand what’s going on. We’re constantly trying to get them to wash their hands, constantly sanitizing, constantly redirecting, and the repetitiveness can be exhausting.
In some cases, family members have pulled their loved one out of our care because they’re nervous about the virus. We’ve been working hard to educate families so that they don’t do this—we don’t want our population going to the hospital because patients 65 or older generally don’t survive when they go there.
For those who we do discharge, we work really closely with all of the home health care agencies so that each person gets three weeks of home health. They’ll get a nurse and a therapist. But a lot of people are declining home health care because they’re scared to have people in their house, and then they’re falling and having to go back to the hospital, so it’s just sad.
Even hospitals are overflowing, so there’s going to come a time where we’re drowning with admissions because patients need somewhere to go after the hospital and nursing homes are some of the only places that will take COVID-19 patients. So even if the virus slows down, nursing homes will still become overcrowded.
It’s been really tough on the staff because we’re the ones who bring the virus into the building; our residents don’t really leave. We’re coming in and can be asymptomatic and are feeling fine and we can be COVID-19 positive and have no idea. It’s hard not to feel guilty.
It’s also been draining because we all have families and don’t want to go home and give it to them. So when you get home you’re strategically trying to take your clothes off, not touch anything, and get right into the shower.
Because the social work department is the heart of where all of the families are calling, we’re constantly getting calls because families have all of these questions. They see things on the news or see our governor speak and then they’re calling and asking ‘Why aren’t you testing? Why aren’t you doing this and that?”
We don’t always have the answers—we’re just going based off of what the Centers for Disease Control and Prevention and the U.S. Department of Health and Human Services is telling us. Clean your areas, wash your hands, all of that stuff. But sometimes you feel like you take 10 steps forward and then 10 steps back.
We have a really good team and our director of nursing acted quickly to manage symptoms in the building so we have a good handle on it. If someone is showing symptoms, now we know exactly what we do.
Last month, we saw a huge decline and didn’t have anyone symptomatic. Then one week went by and we had four people come up positive. So, as cliché as it might sound, we kind of just have to take things day by day.