Dispatches From the Front Lines
Paul Haines graduated in 2018 with a degree in health studies. In July, he will enter his first year at Rowan University School of Osteopathic Medicine. He spoke with us about his experiences working as an EMT during the peak of COVID-19.
I’ve been an EMT for about five years, but I had taken a break from it after I got accepted to medical school. Then the pandemic hit. I was still certified though, so a company that FEMA had contracted to send EMTs to North Jersey reached out to me through LinkedIn. To be honest, I don’t necessarily like being an EMT; being in the ambulance isn’t really for me. But this was during the peak of the outbreak. I realized we are at war with this virus, and I thought that if I could do something to help I should. So I filled out the paperwork and that day headed to the hotel that served as my staging point.
I was stationed in West New York, New Jersey. I had three crew members on my team, and we were one of five ambulances serving the town. At first we worked 24-hour shifts, with 12 hours off to sleep. After there were a few ambulance accidents and the possibility of being immunocompromised with the virus, they changed that to 12-hour shifts.
We were in a hot zone, so basically we were answering calls from the minute we started the shift until the end. We’d get the call, suit up, get to the scene, and put on our PPE before we went into the house. There were a lot of instances where the patients didn’t know if they had to go to the hospital. In many instances they didn’t. They might have had the virus, it just wasn’t severe enough that they needed to go to the hospital to receive care. But almost all of the patients that we did transport had COVID.
In my first week of deployment I helped roughly a hundred patients. About 10% of them died. In my previous experiences as an EMT, less than 1% of my patients died each year. So it was shocking.

I remember one woman in particular. She was in her 60s and had a blood oxygen saturation of 40%. Most people would be dead when it’s that low, but she seemed fine. She was talking and able to stand. We put her on the stair chair to get her down to the street. When we got her outside, I stood her up and remember saying, “Dance with me and I’ll put you on the stretcher.” She was cooperative. But the minute we got her on the stretcher, and the cold wind came by, she coded on us. We quickly got her in the ambulance, started CPR, and transported her to the nearest hospital. When we got her into the ICU, a team of physicians brought her back and intubated her, but she ended up passing away later.
The health disparities of this pandemic are quite obvious. Nearly all of my patients, including that woman, were Hispanic. This virus doesn’t follow any textbooks; it affects everyone differently. I caught it during my deployment but only had a mild case. It started with a cough, and then I developed a 103-degree fever. But after 42 hours of Tylenol and Mucinex DM I was asymptomatic.
I’m fortunate that my family has a second home where I have been able to quarantine. I’ve been here alone for three weeks. I’m awaiting the results of my second COVID test, which I took yesterday. I think it’s probably reasonable to assume that I’m OK given the amount of time I’ve spent in quarantine. But my 96-year-old grandmother lives with my family, so I’m not going home until I know for certain that I’m negative.
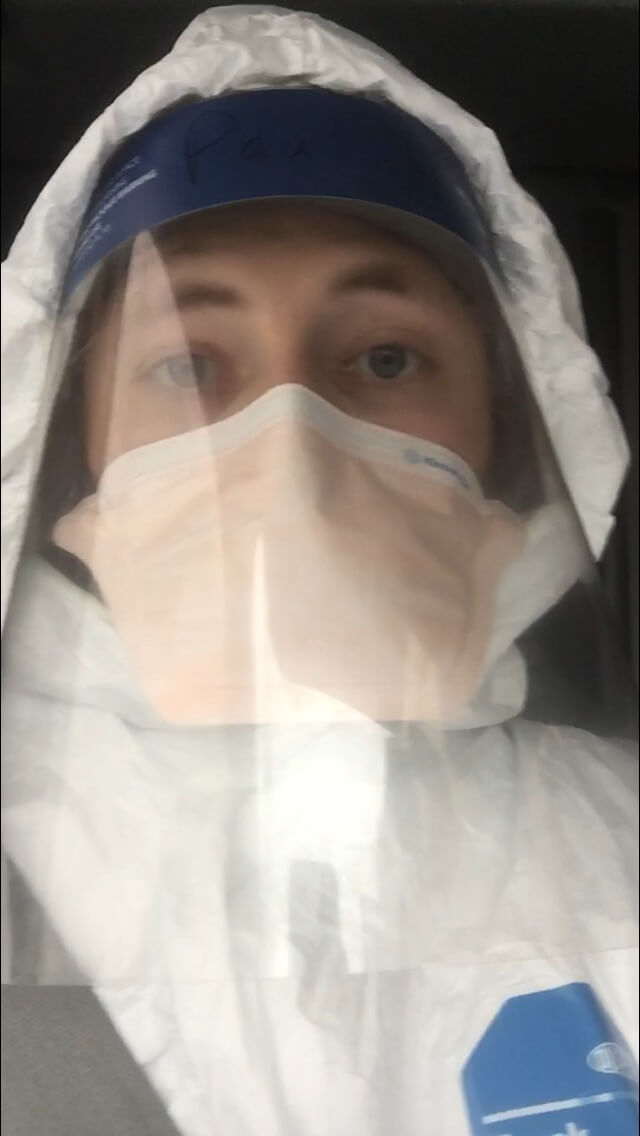
For EMTs, there’s certainly a risk. We’re in a pre-hospital setting, and when you’re walking into closed areas in someone’s house, it’s hard to stay 100% safe. We were given PPE—I had a Tyvek suit, a face shield, a mask, gloves—but whether we all knew how to use it properly is questionable. And we were decontaminating our ambulance ourselves, which was something we hadn’t been trained to do. When Ebola came here, we practiced putting those Ebola suits on. We ran patient simulations. But none of us have lived through a pandemic, so there were a lot of local processes and protocols being done on the fly. Looking ahead, we need to have training simulations in place for EMTs for future pandemics.